- THE 80 MILLION
- Posts
- We’re Back. We’re Still The 80 Million.
We’re Back. We’re Still The 80 Million.
Editor’s Note: It’s hard to know where to re-start the Medicaid dialogue post-passage of Republican’s H.R.1 budget reconciliation legislation. The law makes shocking changes to Medicaid program eligibility and funding that CBO estimates will result in over $1 trillion in federal savings over the next 10 years, primarily because more than one in 10 of the 80 million people enrolled in Medicaid today will lose their health coverage. Acknowledging that most of the close to 9 million people losing Medicaid will lose coverage even though they remain eligible for it, we will remain The 80 Million. Think of us as a benchmark against which you can measure the impacts of H.R.1 and other emerging administrative actions that will cause eligible people to lose Medicaid coverage. Onward.
Speaking of administration actions, today we explain the Trump administration’s recent actions to restrict noncitizens’ access to federal benefits including major health programs. To be clear, Medicaid is not directly affected by these actions, but states, localities, and many providers and non-profit organizations are deeply impacted — ensuring the effects will be felt throughout the health care system.
Authors: Julian Polaris and Elizabeth Dervan
Editors: Patti Boozang and Amanda Eisenberg
Click here to subscribe to receive more content like this!
Help shape The 80 Million: What should we write about next?
tl;dr
On July 10, the Trump administration announced it is expanding restrictions on immigrants’ access to federal programs under the Departments of Health and Human Services (HHS), Agriculture, and Education.
These changes do not directly affect Medicaid, the Children’s Health Insurance Program (CHIP), Medicare or the Marketplaces. However, by restricting access to other health care and social services, these policies are likely to broadly impact the health care system and have downstream effects on these health programs.
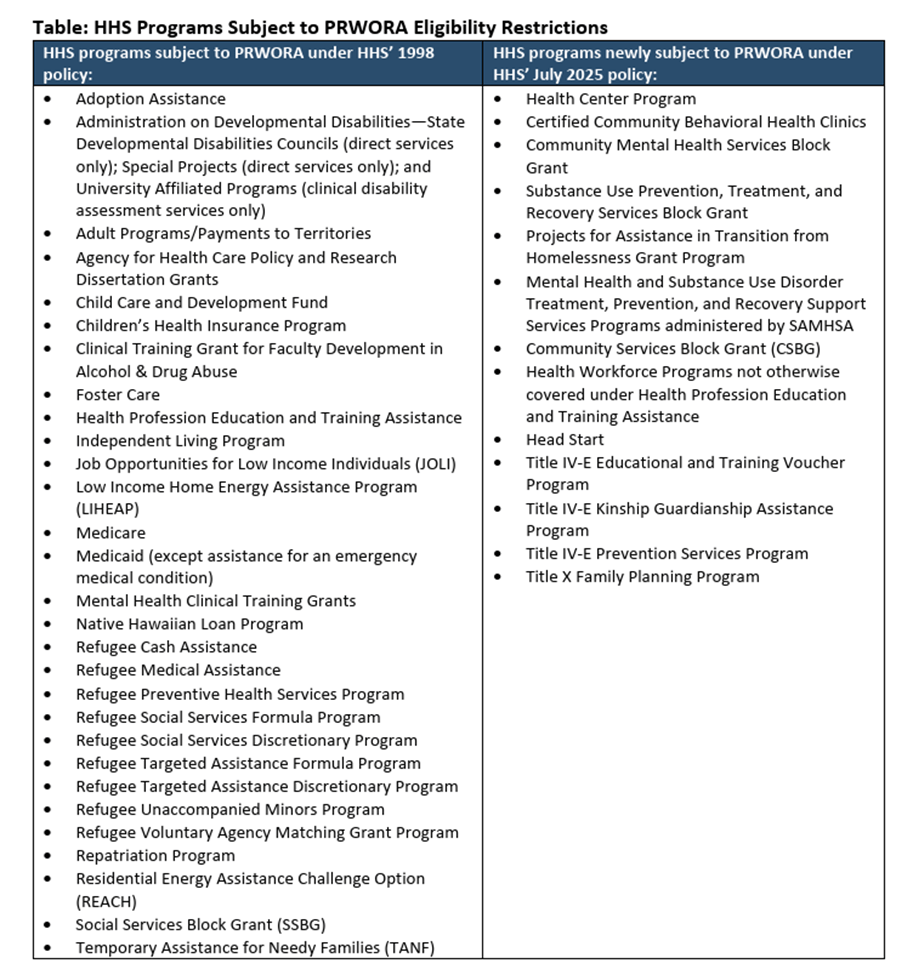
For years, many federal programs (including Medicaid) have been subject to eligibility restrictions for immigrants under the Personal Responsibility and Work Opportunity Reconciliation Act of 1996 (PRWORA). HHS’ announcement expands these restrictions to more than a dozen additional health programs, effective July 14, including funding for community health centers, mental health and substance use disorder services, early childhood education and development, family planning, and other programs. (See the table below for a list of affected programs.)
There are limited exceptions to these restrictions that protect immigrant access to programs related to immunizations, testing, and treatment for communicable diseases; short-term disaster relief; and, under certain circumstances, services delivered by nonprofits. However, effective Aug. 15, the administration has repealed a longstanding exemption for services “necessary for life or safety”— including crisis services and mental health care — pursuant to a recent Department of Justice (DOJ) policy update.
These changes will impact both undocumented and many lawfully residing immigrants. As a result of the expanded restrictions, states, localities and organizations that administer these programs will likely have to begin verifying applicants’ immigration status as a condition of receiving services under many programs, even for programs that historically have not had strict eligibility verifications of any kind.
The 80 Million Impact
Last week, the Trump administration dramatically expanded restrictions for immigrant access to federal health, nutrition, and education programs by redefining the “federal public benefits” that are subject to PRWORA requirements. Recent policy changes will make it harder for many immigrants, including some people who are legally residing in the United States, to access critical health care and social services funded by a variety of federal programs. Questions about these new restrictions abound among stakeholders grappling to understand impacts on patients, health care providers and others on the ground.
These new restrictions mean a much narrower group of noncitizens will be permitted to access impacted federally funded services. As a result, lawful permanent residents (i.e., green card holders) and certain other lawfully residing immigrant groups will now face a five-year waiting period to receive certain means-tested benefits. Undocumented individuals will become ineligible entirely for these programs, as well lawfully present individuals with work visas, student visas or pending asylum applications.
HHS has announced that effective July 14, immigrant eligibility restrictions in PRWORA newly apply to over a dozen additional programs that fund a broad array of important health care and social services. Newly impacted programs include certified community behavioral health clinics, mental health and substance use disorder programs administered by the Substance Abuse and Mental Health Services Administration, Title X family planning services, funding for community health centers, and Head Start Programs (see the Table below for a list of affected programs). Among other rationales, HHS asserts that PRWORA’s restrictions apply to most federally funded benefits received at the individual, family, or household level.
Historically, HHS had interpreted PRWORA as not applying to programs that lacked other, non-immigration related eligibility criteria (such as income limits), nor to programs funding early or K-12 education. In addition to listing a number of programs that are now subject to PROWRA, HHS’ new guidance warned that its list was not exhaustive, and that additional programs could be announced in the future.
Existing statutory exemptions will protect noncitizens’ access to certain services, including short-term disaster relief as well as immunizations, testing and treatment for communicable diseases — potentially protecting programs focused on HIV/AIDS, sexually transmitted diseases, and vaccines. However, in a separate policy announced by DOJ, the administration is ending a longstanding exemption for services “necessary for life or safety,” effective Aug. 15. For decades, this exemption has protected access to services such as grant-funded crisis intervention, mental health and substance use disorder care, soup kitchens and meals on wheels, and short-term housing for the homeless, victims of domestic violence, and abused or abandoned children.
Taken together, the administration’s dramatic expansion of PRWORA’s restrictions and repeal of longstanding protections for life-saving services will have severe consequences for immigrant communities and public health, likely producing chilling effects that could lead eligible family and community members (including citizens) to forgo care.
Stakeholders who operate these federally funded programs are puzzling through what all of this means on the ground. The first question is which specific activities are now subject to PRWORA restrictions. Even within the programs HHS has identified as subject to PRWORA, certain activities may remain unaffected, whether because they qualify for an exemption (e.g., related to communicable diseases), or because they are delivered without a focus on benefits for individuals, families, or households, such as weatherization for multi-unit buildings (an example cited in HHS’ guidance).
For benefits subject to PRWORA, program administrators will likely have to verify immigration status before providing services by checking self-attested immigration status against federal databases. This could mean significant operational challenges and run counter to the mission and clinical evidence for programs like crisis lines where asking about eligibility impedes intervention for people in life-or-death circumstances.
Importantly, nonprofits are generally exempt from conducting these types of verifications, though states and others may still be required to verify immigration status even if they provide subawards to nonprofits for service delivery (which could have implications for how those nonprofits deliver services). The administration could (and is expected to) change this nonprofit exemption down the road, further complicating this picture.
While HHS’ announcement does not impact Medicaid or CHIP, these changes will be felt throughout the health care system as immigrants face higher barriers to care and social services, and as chilling effects potentially dissuade eligible immigrants and family members from seeking services. Combined with H.R.1’s scaling back of Medicaid and CHIP eligibility for many immigrants, the result will likely be delayed care, worse health, and more frequent and expensive emergency care at emergency rooms (paid for, frequently, by Medicaid). States will also need to contend with more eligibility verifications and potentially different complex eligibility requirements across different programs.
The Bottom Line
Overall, these recent actions reflect another step in the administration’s broad agenda to target noncitizens’ use of federal programs. HHS’ updated PRWORA policy will likely have profound implications for immigrant communities, the state and local government agencies and private entities that administer federally funded programs, health care providers, and overall public health. More immigrants, including lawfully residing individuals, will be denied access to health care and social services that have long been available to them. New restrictions may cause confusion or chilling effects that lead eligible immigrants to forgo federally funded services. Entities administering these federal benefits and programs will likely need to adopt new procedures and update their IT systems to verify individuals’ status. Additional policies and announcements are likely to come in the months ahead.
Help shape The 80 Million: What should we write about next?